Background
Danilo Miskovic is a consultant colorectal surgeon specialising in training and robotic surgery for colorectal cancer at St Mark’s Hospital and the London Clinic. He is a Swiss national and his undergraduate education was in Zurich. He gave us an insight into his background and explained how he came to work in the UK before discussing the specifics of his current work as a consultant colorectal surgeon.
He spent his early years in a rural village in the eastern part of Switzerland. His father, also a doctor, is Serbian and had moved from Croatia as a Yugoslavian soldier in WWII to Switzerland after qualification. Danilo’s Swiss mother was a professional artist.
The family moved to Zurich when he was 7 years old to benefit from the much better education on offer there.
Confessing that he wasn’t exactly a model student (just like his blogger father-in law), he was handed an underwhelming reference from the Dean, and his plan to go to the States was trumped(!), in favour of a spell working in the Solomon Islands. Here he learned how to cope with very limited available resource, an ideal experience for his subsequent future in our own NHS.
After basic surgical training he arrived at Frimley Park Hospital in Surrey on an exchange fellowship. Your blogger was also at Frimley during the Falklands War as a trainee surgeon and witnessed the first of a generation of Swiss surgeons coming there year after year. Always a “plan A” opportunist, Danilo signed on for a PhD in surgical training data management at Imperial College, paving the way for his later specialist posts at Portsmouth, Leeds and St Mark’s, gaining experience in minimally invasive (laparoscopic or keyhole) surgery for colorectal cancer.
St Mark’s Hospital
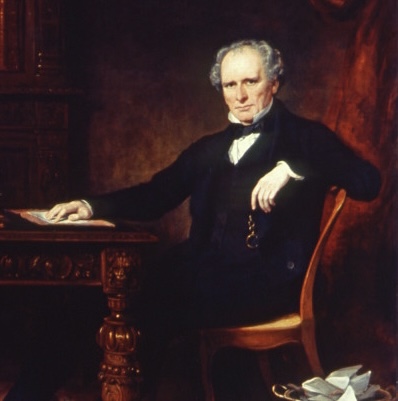
Danilo gave a short history of St Mark’s Hospital, which was established in Aldersgate Street in 1835 by Frederick Salmon
and had the grand title of “The Infirmary for the Relief of the Poor Afflicted with Fistula and other Diseases of the Rectum”. The hospital moved to City Road London in 1896 and finally to Northwick Park, Harrow, as The National Bowel Hospital, delivering high quality education, innovation, research and treatment for medical and surgical gastrointestinal disease. It serves as a public hospital for the local population but its main business is tertiary clinical care for difficult cases from around the UK and overseas. It also has a very successful Research Foundation, a worthy cause for any Probus member thinking of disbursement www.stmarkshospitalfoundation.org.uk
Development of Minimally Invasive Surgery (or keyhole/laparoscopic surgery)
Danilo’s whistle-stop tour through surgical history focussed on technical skill. Back in the Middle Ages they shared and overlapped practice with the barbers; blood-letting, cupping, amputations, beard trimming and haircuts. They amalgamated to form the barber-surgeons, whose guilds still exist in London and elsewhere. There was a degree of public entertainment and also demonstrating to other surgeons
The crucial development for modern surgery was defined by the introduction of anaesthesia, which removed the pain element, to allow time for precision operating. No need now to take a leg off in 4 minutes flat. Precision operating has had a huge impact on complications and long-term survival.
Minimally invasive surgery has been refined continuously since the 1990s, resulting in much less trauma and faster recovery of the patient compared with open traditional surgery.
Procedures are increasingly standardised and automated, with much more patient involvement now in operation choice and postoperative follow up.
Bowel cancer
Colorectalcancer can occur anywhere along its length but the risk of spread is worse with right sided cancers. The reasons are not fully understood but age, genetic (family history) and environmental (e.g. dietary) factors are responsible. Adjusting and individualising the operation for right-sided cancers may well be able to correct any survival disadvantage in the future. Robotic surgery lends itself very well to this challenge.
Danilo restricts his time to the investigation and treatment of bowel cancer and he leads a large robotic team at St Mark’s. Laparoscopic surgery, for many years the domain of the gynaecologist, has been shown to result in faster recovery and better long-term survival of patients with colorectal cancer, but is very skill dependent. A major problem was the long learning curve for surgeons undergoing training, often those who were older, less computer-game savvy, experiencing the transition from conventional operating using long painful incisions, but also worth mentioning here that there are still complex operations today which just can’t be done by keyhole. Without formal training by oneself it was claimed that it would take an average of 150 cases to achieve keyhole surgery proficiency. A National Training Programme using “fresh” cadavers was introduced, the younger “play-station“ generation teaching the older traditionally-trained surgeons (as per your blogger), a true paradigm shift. As time went along, the National Training Programme, improved instrument technology and video resolution dramatically shortened the learning curve and patient outcomes. These procedures are tightly regulated nationally.
Robotic Surgery
Robotic surgery was introduced in the early 2000s.
A single robot is expensive, equating to the cost 50 family cars. An industrial robot can be fully automated, but this is not the case with surgery. The surgeon always stays in control, manipulating the instrument stack from a console in the operating theatre but remotely from the patient (.
The instruments are introduced into the patient’s abdomen to access and remove that part of the colon containing the cancer with its associated blood supply and lymph glands. Access ports are inserted through 1cm or so pre-marked incisions.
The instruments exactly reproduce the movements of the surgeon’s hands and even more precision is obtained by scaling down the image. Any slight tremor that any of us might get is obliterated by this fantastic technology. But it’s just a tool which can’t do the surgery itself for you and success depends entirely on the surgeon’s skill, the patient’s own risk factors e.g. obesity, heart disease and the large supporting team. But human error can never be completely avoided, as elsewhere in life. The reassuring thing is that robotic failure is extremely rare. A real advantage is that obesity and restricted space are easier to access with the robot.
Surgical training is not the same as in the airline industry, where simulators are a great teaching tool. With human anatomy so variable, how can the surgeon predict such variability to improve the patient’s outcome in surgery? At St Mark’s, 3-D computer generated models constructed for individual patients
are based upon the patient’s own scans, defining and guiding where to negotiate the anatomy within the abdomen, and more importantly where not to go. Computerised tomography (CT scan) images are superimposed on the real-time operating video image viewed by the operating surgeon in theatre, who is then readily able to identify any anatomical anomaly and avoid trouble. This integrated model is rather like a sat nav in the car, telling you exactly where to go. Fortunately the robot is far more accurate than sat-nav. But understanding anatomy is crucial and there’s a worry these days that study of anatomy has been significantly diluted in medical schools in the UK.
Andrew Shorthouse
11 March 2022
Fig 1 Danilo Miskovic PhD FRCS (the Blogger’s portrait)
Fig 2 Frederick Salmon, founder of St Mark’s Hospital London
Fig 3 The Quack (c 1785) F A Maulbertsch
Fig 4 Robot instrument stack and operating surgeon seated at the remote console
Fig 5 Arterial clips prevent bleeding after the colon tumour blood supply has been divided and before removing the affected segment of colon. Integrated imaging, shown in the inset, provides detailed real-time operative guidance, especially useful if there is any anatomical anomaly